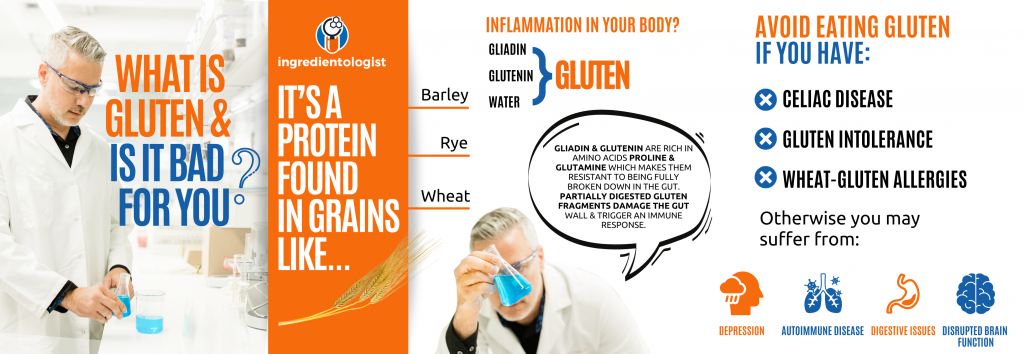
Although most government guidelines in the USA and Europe advise people to eat adequate amounts of grains each day, it’s important to know that these grains often contain ‘antinutrients’ such as gluten and lectins that can cause disease and unwanted symptoms in humans. Gluten is a general term for a group of structural proteins found in wheat (prolamins and glutenins). It is also found in other grains like barley and rye, and is what gives bread its dough-like, fluffy texture and is also added to many other foods to create a more desirable consistency. As a result, it is used as an additive to many products in the food and beverage industry making it difficult to avoid completely.
Unfortunately, gluten is responsible for causing several intolerances in humans, most severe being celiac disease which is an autoimmune disease of the intestine. Slightly less severe is non-celiac gluten sensitivity (NCGS); a related gluten disorder which triggers an immune response but is not an autoimmune condition. When gluten interacts with the cells lining the intestine, it triggers the immune system to respond, causing inflammation and damage to the gut. When this trigger remains, and the immune system is continuously activated, the inflammatory response can become chronic or long-lasting.
Both celiac disease and NCGS cause gastrointestinal and extraintestinal symptoms that are similar, and adherence to a strict gluten-free diet is the primary treatment in both cases. Adhering to a long-term gluten-free diet can be challenging as wheat and many other gluten-containing grains are a primary component of our diets today.

CELIAC DISEASE
Nowadays, the word ‘celiac’ gets thrown around a lot with little understanding of the pathophysiology behind celiac disease (CD) and the seriousness of its effects. Celiac disease only occurs in people who have a particular set of genes that produce certain molecules that recognize parts of gluten proteins and stimulate an immune reaction. Gluten is also responsible for other disorders such as non-celiac gluten sensitivity (NCGS) and wheat allergy, but CD is the most prevalent and severe of all.
Celiac disease is a gluten-induced chronic inflammatory enteropathy (disease of the small intestine).1 To put that in simple terms, it is a disease caused by an intolerance to gluten where certain parts of the gluten proteins are recognized by the body’s immune cells as ‘toxic’ causing them to launch a very specific immune response that results in damage and inflammation to the intestinal lining in genetically susceptible people. This damage to the gut causes gastrointestinal symptoms as well as poor absorption of nutrients from foods. But, extraintestinal symptoms such as headaches, skin issues, brain fog, fatigue and muscle weakness are also seen.1
Two of the major factors influencing the disease are environmental and genetic factors. This means your genetics as well as your exposure to gluten and other toxins can influence your risk of developing CD.
- Environmental factors: Gluten exposure during childhood, especially during the first year of life, can influence one’s susceptibility and even the type of milk and length of breastfeeding are both potential triggers for the disease.2
- Genetic factors: A particular set of genes that produce a certain protein called human-leukocyte antigen (HLA) DQ 2 or DQ 8 is associated with CD. If you have either one of these genes, you’re more likely to have the disease. This means that your cells express the ‘HLA complex’ which is suggested to bind strongly to gluten, presenting gluten to our immune cells which go on to cause an inflammatory immune response in the intestine.2
THE MECHANISM OF ACTION
Gluten is a complex mixture of proteins found in cereal grains known as prolamins of which the main proteins are glutenin and gliadin and both have been implicated in causing gluten intolerance. These proteins are the storage form of starch for seeds, providing the sprouting seed with the nutrients it needs to grow. Scientists have uncovered many different but related structures of these gluten proteins. It was initially believed that only certain structures of glutenin or gliadin were toxic or immunogenic (causing an immune response), but now we know that almost all of them could be triggers. What’s more, is that different people may react to different gluten structures, and so identifying the exact mechanism behind gluten-related disorders is a challenge!3
As a side note, this is the basis as to why certain wheat varieties can be more ‘harmful’ to celiacs than others. In any given wheat variety, there exists over 100 unique gliadin and glutenin structures. The amount and type of gluten in wheat, and other grains, has evolved over the years with more modern wheat varieties being genetically modified. Ancient wheat species known as ‘diploid’ have given rise to new ‘tetraploid’ and ‘hexaploid’ species through natural hybridization/cross-breeding.3 These new varieties have a different set of genes that give the wheat larger amounts of gluten, making them more desirable for commercial purposes. As new structures of gluten proteins emerge as a result of modern agricultural practices, more immune-stimulating gluten peptides are found in foods.
Getting back to the mechanism of action, these gliadin and glutenin proteins are made up of certain amino acids with particularly high amounts of proline and glutamine. Their unique structure is what makes them resistant to proper digestion by any of our stomach enzymes and as a result, we can’t break them down into individual amino acids, as we would with other proteins. Large protein fragments (called peptides) of gluten end up in the intestine and in susceptible individuals these peptides are what trigger an immune response, inflammation and cause damage to the gut lining.1,3
When the peptides described above come into contact with the cells of the intestinal wall, they damage the cells lining the gut, increasing gut permeability. A protein, called zonulin, which regulates the tight junctions – the gaps between the cells lining the gut – is increased. Zonulin disrupts the integrity of the tight junctions, making them ‘loose’ allowing the movement of gluten peptides passed the gut barrier. It’s as if someone were poking holes in your intestinal wall making it a poor barrier between the food you’re eating and your bloodstream. This is what we know as ‘leaky gut syndrome’.
Now, these large gluten fragments can leak into the bloodstream that normally wouldn’t and once here, they bind to specific molecules called ‘HLA-DQ 2/DQ 8 receptors’ which are present in people who carry the genetic code for them. Gluten fragments are negatively charged, while the HLA-DQ 2/DQ 8 receptors are positively charged and so they bind very strongly. This bond then triggers immune cells (CD4+ T-cells) to start secreting many proinflammatory substances and antibodies.1,2
Another gluten-related disorder is non-celiac gluten sensitivity (NCGS) which is a clinical term used that describes the adverse gastrointestinal (GI) or other symptoms experienced after gluten ingestion, although is not associated with the same degree of immune activation or gut damage. There is a lot of controversy around whether NCGS is truly different from irritable bowel syndrome (IBS) or CD due to their overlapping causes and symptoms. Some experts suggest that NCGS may be caused by other dietary triggers found in gluten-containing foods such as allergens in wheat, amylase trypsin inhibitors (ATIs), lectins and FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides and polyols). While FODMAPs are present in gluten-containing grains and have been identified to cause GI distress, such as bloating, they likely aren’t the cause of the extraintestinal symptoms, like headaches, fatigue and eczema, seen in NCGS. People who remove gluten from their diet still eat foods containing many FODMAPs, like fruit. The many unknown variables and lack of clear biomarkers makes identifying NCGS a challenge, and proves to be more complicated than CD.4
Approximately 1% of the global population has CD, and the prevalence is increasing. The disease can occur at any stage in life but peaks mainly during childhood (less than 6 years old) and in one’s 40’s or 50’s.5 On the other hand, the prevalence of NCGS has been reported to be anywhere between 0.63 and 6.0%.6
CD VS NCGS
The main difference between CD and NCGS is the response of the immune system to gluten coming into contact with the gut lining. Celiac disease is an autoimmune disease where gluten triggers the adaptive immune system. This is seen by antibody production by your own T-cells which act as signaling molecules that tell the immune system there is something that needs to be destroyed. Immune cells continue to be produced that attack the cells lining your intestine, causing inflammation and damage to the cell wall.1,6
In contrast, NCGS is an innate immune response to gluten seen by a rise in innate immune cells and an absence of any gluten-related antibodies. Unlike the adaptive immune system which confers long-term memory for future antigen exposure, the innate immune defense is our first line of defense and doesn’t provide long-term immunity towards a particular toxin.1,2,6
SYMPTOMS
Both CD and NCGS display gastrointestinal (GI) and extraintestinal symptoms. Symptoms can appear within days to weeks in CD patients and within hours to weeks with NCGS patients.
The table below summarises the symptoms related to NCGS, while those with CD experience similar symptoms. The severity of the symptoms depends on the individual entirely.
Table 1 Non-celiac Gluten Sensitivity GI & Extraintestinal Symptoms
| Gastrointestinal | Extraintestinal |
| Bloating | “Foggy” mind |
| Diarrhea | Tiredness |
| Constipation | Fatigue |
| Abdominal pain | Joint pain |
| Nausea | Depression |
| Vomiting | Numbness |
| Anal fissures | Loss of balance |
| Eczema | |
| Anemia | |
| Weight fluctuations | |
| Rash | |
| Headaches |
In addition to the above symptoms, CD patients can experience more severe forms of diarrhea and abdominal bloating, delayed growth, thyroiditis and even infertility.7
DIAGNOSIS OF CD AND NCGS
To determine whether someone is celiac or not, tests for the presence of certain antibodies in the blood called immunoglobulin A (IgA) and immunoglobulin G (IgG) can be done, which is then confirmed with a genetic test for HLA DQ 2 or DQ 8. A tissue sample of a person’s intestinal wall is also taken and the extent of damage is evaluated with a grading system.
In contrast, there are no blood biomarkers that help us identify NCGS, and there is not much known about what causes NCGS exactly. Typically, it is determined by ruling out CD (absence of celiac-specific antibodies and a negative genetic test) in those with a gluten sensitivity who show gastrointestinal or extraintestinal symptoms, and whose symptoms improve following a gluten-free diet. Additionally, while those with CD display damage to the lining of the intestine, those with NCGS typically don’t.1,6,8
Because of their similarity, clinicians can’t differentiate between CD and NCGS based on symptoms alone, so these tests need to be done and should be done before implementing a gluten-free diet because testing after this can give inaccurate results.8 Most doctors will recommend a gluten challenge prior to testing, which means eating gluten to ensure it is present in your body before getting a test.
If you’re experiencing symptoms, but do not think it is gluten, you may have a wheat allergy. This can be confirmed by detecting IgE by a simple skin prick test and symptoms are usually seen within minutes or hours. An allergic response to wheat is different from the autoimmune or innate immune responses seen in CD and NCGS, respectively.8
CONDITIONS ASSOCIATED WITH CELIAC DISEASE
Many disorders appear to be associated with celiac disease with most being either genetic, autoimmune or neurological. Individuals with the following diseases have a greater risk for CD:
- Type 1 Diabetes
- Autoimmune thyroid disorders
- Autoimmune hepatitis
- Neurological disorders such as epilepsy
Gluten appears to worsen autoimmune conditions such as Hashimoto’s, rheumatoid arthritis and type 1 diabetes. This is because the underlying mechanism is the same in which the body’s own immune system identifies a foreign antigen (a substance that triggers an immune response) that shares similarities with your body’s own antigens. The result is an immune response to both the ingested antigen and your body’s own tissues.
Other conditions that gluten appears to worsen are bowel diseases such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). These diseases are tied to the integrity of the gut lining and avoiding gluten appears to improve these conditions.
TREATMENT
Gluten-free diets remain to be the gold standard treatment for celiac patients as well as those with gluten sensitivity. Sticking to a gluten-free diet for life can be challenging and requires a significant amount of energy and effort, especially with the excessive amount of processed foods today. Many celiac patients also report negative psychosocial effects due to the restrictive nature of the diet.
Studies have shown that 20-38% of celiac patients have some degree of nutritional deficiency whether it is total calories, protein, fiber, vitamins or minerals. It is unclear whether this occurs because of the disorder or because of the restrictive nature of a gluten-free diet. A nutrient deficiency is caused because of the damaged intestinal wall. Malabsorption of nutrients like B vitamins, iron, calcium and vitamin D in the small intestine is common and the degree of intestinal damage and the length of time following a gluten-free diet are factors that would influence how nutrient deficient someone is. Many gluten-free foods contain processed grains where the outer fibrous layer is removed, which lowers the fiber intake of anyone on a gluten-free diet. However, if fibrous vegetables, nuts and seeds are prioritized on a gluten-free diet, low fiber intake can be prevented.
In addition to actively avoiding gluten, there are alternative ways to decrease gluten’s impact on those with a gluten sensitivity. For example, there are some supplements you can take that help your body metabolize gluten slightly better.
SUPPLEMENTS
As discussed, gluten is a protein, just like other proteins we get from the foods we eat as it consists of many amino acids that make up the whole protein. But, in the case for people with a gluten intolerance, their bodies can’t break down this protein properly. Gluten is only partially digested or not digested at all, which causes it to have negative effects in the small intestine.
There are gluten-digesting supplements that you can buy which contain certain enzymes that can break down the gluten protein by breaking the bonds between the amino acids of the gluten protein fragments in the stomach, before it reaches the small intestine where it can cause damage. These particular enzymes can break the proline and glutamine rich amino acid bonds.
Some examples:
- Gluten Guardian by BiOptimizers
- Gluten Digest by NOW
- Gluten Rescue by Doctor’s Best
The use of certain strains of probiotics is also widely used to treat CD. These probiotics can ferment and degrade gluten proteins in the intestine into protein fragments that are no longer immunogenic. These probiotics can also improve the nutrient absorption in the gut and improve the overall gut microbiome.
Taking supplements to metabolize gluten while indulging in a gluten-containing meal, or following a standard american diet that is high in gluten is not recommended for someone who has CD. These supplements are definitely not a good long-term solution. However, they can be useful for when the risk of gluten exposure is high – for example when traveling or eating out.
MODIFIED GRAINS
Scientists can breed certain types of wheat varieties with a more favorable ‘toxicity’ profile by selectively breeding early wheat species or by genetically engineering them to have silenced gluten proteins, but none will be completely safe for celiacs. However, this is not widely done as removing the gluten proteins from wheat will take away the very properties that make it suitable for production, and there are many regulations regarding genetic modification of plants that need to be considered.10
Other treatments such as immunotherapy and vaccines are being investigated and as scientists progress in the research in this field, more solutions will become available to celiacs.10
You may think that whether you have CD or NCGS that it does not matter, as treatments are similar, but in the case for celiacs, symptoms are far more severe and frequent exposure to gluten can lead to nutritional deficiencies and other possible comorbidities. Let’s take a look at how to best navigate a gluten-free diet!
GLUTEN-FREE DIETS/FOODS
Many diets have come and gone over the years, but the gluten-free diet is here to stay. Being the primary treatment for anyone with gluten intolerance, this diet won’t disappear like the other weight-loss fads. While it’s used clinically, people have started to adopt a gluten-free diet with the perception of it being healthier than a regular diet. In fact, there are so many people that aren’t even gluten sensitive and follow a gluten-free diet that there’s a name for this population. They’re called PWAG for ‘people who avoid gluten’ and there are studies being done on them!
Anyone who is celiac, or has a friend or family member who is celiac can agree that a gluten-free diet can be difficult. Going out to restaurants without interrogating the server like a detective just isn’t possible, and shopping at the supermarket is no easy task, with gluten appearing in almost everything. On top of that, people are always warned about a gluten-free diet being restrictive and causing nutrient deficiencies. Well, that’s not wrong, but sadly it is only because people are searching for the label that says ‘gluten-free’ on processed food options, instead of looking for foods that are naturally gluten-free.
With the marketing claims of many big brands, we are often misled to believe that something with a ‘gluten-free’ label on it is somehow healthier for us. Previous studies that have taken a look at the nutritional composition of gluten-free products found that they contain high amounts of fat, sugar and salt.11 Now, recall that eating fat and sugar together is a recipe for inflammation, glycation and oxidation in the body – all which lead to weight gain and poor metabolic health. On top of that, people adhering to a gluten-free diet don’t meet the recommended calcium, iron and fiber intakes. Overall, adults who follow gluten-free diets are not eating enough nutrient-dense foods to meet all nutritional recommendations.10,11,12
WHY MANY PEOPLE FEEL BETTER AVOIDING GLUTEN
Actively removing gluten from your diet probably means you’re going to be skipping many of the processed, packaged foods like breads, cereals, snack bars, and candy which are typically higher in calories, sugar and unhealthy fats. Of course, many people tend to lose weight and even improve things like joint pain, fatigue or other health issues when they avoid gluten. This is likely because of fewer refined carbohydrates and sugars in their diet. Also, digestive issues can disappear as FODMAPs are reduced which are carbohydrates that don’t get digested but get fermented by bacteria in the colon and can cause bloating and gas in susceptible people.
While many may benefit from a gluten-free diet, those who don’t focus on diet quality may be harming themselves.9,10According to a study that looked at the effects of a gluten-free diet on non-celiac people, there are potential harms caused by the diet such as11:
- Deficiencies of micronutrients & fiber
- Increased (poor quality) fat content
- Hyperlipidemia
- Hyperglycemia
- Coronary artery disease
- Increased financial costs
- Social restrictions
Paradoxically, in many cases, following a strict gluten-free diet could be detrimental to a celiac’s nutritional health because of the poor quality nutrition it can provide. That said, if you’re not celiac, you probably don’t want to put yourself on a gluten-free diet as there are many other alternatives like a paleo or ketogenic diet that may not come with the negative side effects.
THE BEST DIETS TO FOLLOW:
- Autoimmune Protocol
- Primal diet
- Paleo diet
- Ketogenic diet
- Carnivore diet
- Whole 30
- Low-carb
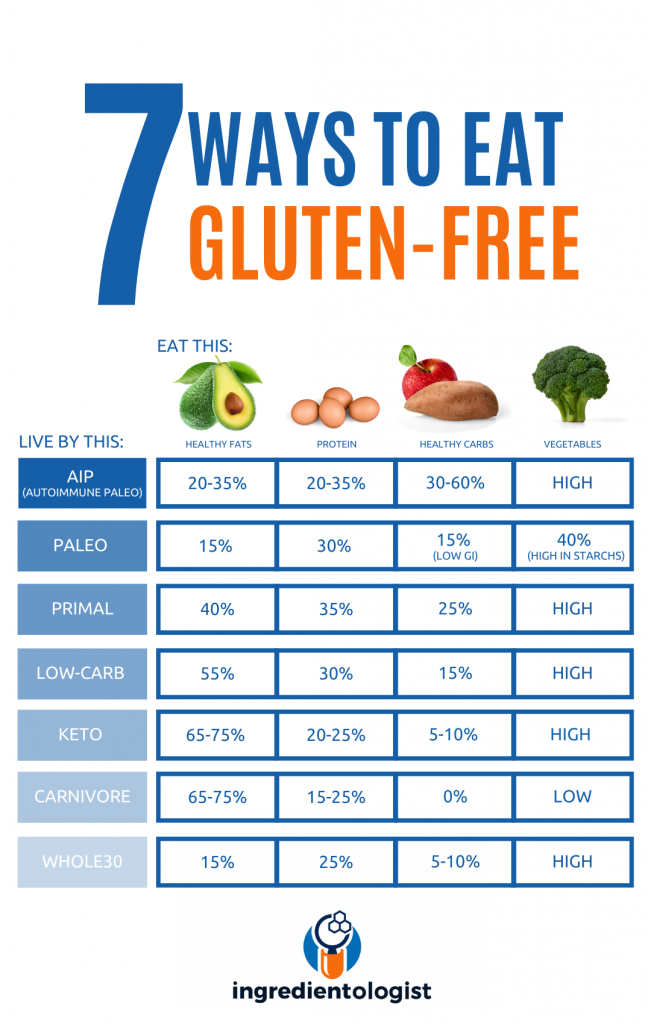 Although these diets vary in their limitations, most of them focus on limiting antinutrient intake, which can help reduce your exposure to gluten significantly. All of these diets are whole-foods focused which means they exclude processed products that contain highly-refined carbohydrates, sugars and additives. While the AIP diet is specifically targeted at autoimmune diseases, such as CD, it is a good place to start. Start your gluten-free diet as strict as possible and slowly reintroduce some food groups into your diet that may be potential triggers for your unwanted symptoms. The key to success here is self-experimentation, as no individuals are exactly the same in what they are sensitive to.
Although these diets vary in their limitations, most of them focus on limiting antinutrient intake, which can help reduce your exposure to gluten significantly. All of these diets are whole-foods focused which means they exclude processed products that contain highly-refined carbohydrates, sugars and additives. While the AIP diet is specifically targeted at autoimmune diseases, such as CD, it is a good place to start. Start your gluten-free diet as strict as possible and slowly reintroduce some food groups into your diet that may be potential triggers for your unwanted symptoms. The key to success here is self-experimentation, as no individuals are exactly the same in what they are sensitive to.
GLUTEN-FREE FOODS
Gluten is found in many grains such as wheat, barley and rye. In the culinary industry, gluten is used to give food elasticity and moisture and it is what makes bread rise and gives it a chewy texture. These effects have made gluten a very desirable protein to be added to many foods. Better taste, texture and quality means more sales – it’s a no brainer!
Gluten-containing foods are a major component of the current Western diet and adhering to a gluten-free diet can improve the symptoms experienced by those with CD or NCGS. Improvements can be seen within a few weeks and the damage to the gut wall can take 1-2 years. A gluten-free diet doesn’t heal someone with CD, but it can improve their quality of life significantly.
Let’s take a look at some food categories and identify the foods that you can eat on a gluten-free diet. Unfortunately, nowadays it is not as simple as excluding wheat, barley and rye as many boxed and packaged foods have added gluten and gluten-free grains can be contaminated with gluten during production.
WHOLE GRAINS:
Surprisingly, there are a few grains that you can eat on a gluten-free diet. They may be less common and oftentimes more expensive. Many grains are naturally gluten-free, but some can get contaminated during processing. For example, oats are often processed in the same facility as wheat making cross-contamination possible, so make sure you look for certified gluten-free oats. Gluten-free grains include:
- Brown rice & wild rice
- Quinoa
- Buckwheat
- Sorghum
- Tapioca
- Millet
- Amaranth
- Teff
- Arrowroot
- Oats (labelled gluten-free)
 Sourdough Bread: Bread made with gluten-free flours is optimal for those with celiac but research has shown that gluten proteins can be degraded by the bacteria and yeast during sourdough fermentation to the extent that sourdough breads may be more tolerable for some with a gluten sensitivity. Use a starter culture to make your own bread at home or look for artisanal bakeries that use traditional baking techniques.
Sourdough Bread: Bread made with gluten-free flours is optimal for those with celiac but research has shown that gluten proteins can be degraded by the bacteria and yeast during sourdough fermentation to the extent that sourdough breads may be more tolerable for some with a gluten sensitivity. Use a starter culture to make your own bread at home or look for artisanal bakeries that use traditional baking techniques.
FRUITS & VEGETABLES:
All fruits and vegetables are naturally gluten free, however be cautious when buying things like canned, frozen, dried or pre-prepared fruit/veg as they can contain thickeners or flavoring that can contain gluten. Look out for:
- Maltodextrin
- Malt extract/vinegar/syrup
- Modified food starch
- Textured vegetable protein
- MSG
- Citric acid
- Hydrolyzed plant protein
- Some natural & artificial flavors
- Emulsifiers
PROTEINS:
Grass-fed meat, pasture-raised eggs and wild-caught fish are the best sources of protein and are gluten free. But, nowadays we tend to buy many pre-packaged proteins that contain marinades or sauces that contain malt vinegar, flours or soy sauce. Processed meats like sausages and salami should be avoided and vegetarian burger/meat sources almost always contain some gluten. Proteins that are safe to consume include unprocessed:
- Red meat
- Chicken
- Seafood
- Tofu, tempeh & edamame
- Nuts & seeds
- Beans & legumes
DAIRY PRODUCTS:
As with protein sources, most dairy products are naturally gluten free but when they’re processed, flavoring, thickening and stabilizing agents are added which may contain gluten. You can include all dairy products, but double check the labels when it comes to the following:
- Flavored & sweetened yoghurts/milks (especially if added granola/fruit pieces)
- Processed cheese (usually fine, but check the label)
- Dairy desserts like ice cream and frozen yogurt
Dairy is known to cause gastrointestinal issues due to lactose intolerance in some people, and those with gluten sensitivity are more likely to be lactose intolerant. Avoiding dairy products for the beginning phases of your gluten-free diet is a good idea while closely monitoring your symptoms when reintroducing dairy back into your diet.
SPICES, SAUCES & CONDIMENTS:
Naturally gluten-free options include:
- Coconut aminos
- Tamari sauce
- Apple cider vinegar & white vinegar
Commonly overlooked, spices, sauces and condiments often have gluten added to them. In particular look out for maltodextrin, malt, modified food starch and wheat flour.
Read the labels of the following carefully:
- Rice vinegar
- Marinades
- Ketchup, mustard, mayonnaise
- Stocks
- Dry spices
- Gravy mixes
- Also check cooking oil sprays, and flavored oils
BEVERAGES:
Most drinks are gluten free, but it’s a good idea to check flavored syrups, mix-in powders and ready-to-drink products. Alcoholic beverages to avoid include beers made from gluten-containing grains and malt-based beverages. Distilled liquor like vodka, gin and whiskey can sometimes trigger celiac symptoms, but wine, some ciders and gluten-free beers are tolerated.
As some nutrient deficiencies like iron, calcium and vitamin B are common among celiacs adopting a gluten-free diet, I recommend testing your nutritional status regularly and to supplement where necessary. But, meat, eggs and many vegetables can provide more than enough of these nutrients too.
IN SUMMARY
For the celiacs out there, going gluten-free doesn’t have to be that hard! By sticking to the golden rule of eating whole foods as much as possible, life becomes a whole lot easier. Learn how to read your nutrition labels and look out for the risky ingredients mentioned above. Anything that comes in a box or packaging is not only increasing your risk of gluten exposure significantly, but also making a nutrient deficiency far more likely because these processed foods are stripped of their nutrients.
In fact, a gluten-free diet can actually be played to your advantage. You’re forced to avoid foods that are high in refined carbohydrates which are often processed, contain added sugars and provide minimal nutritional value. Most bottled sauces, pre-made meals, breads and cakes are also eliminated, which is definitely a good thing for the waistline and your long term health. A shift in focus towards natural, whole foods is the easiest way to to limit gluten exposure, and funnily enough, is often the healthiest and most nutrient-dense diet.
If you suspect gluten intolerance, but don’t want to mess with any testing, why not try going gluten-free for a period of time and slowly reintroduce foods back into your diet. As long as you replace gluten-containing foods with nutritious foods, cutting out gluten won’t cause any adverse health effects. I follow a ketogenic diet most of the time and because I’m limiting my intake of any sort of carbohydrates, I’m almost completely gluten-free. There are many swaps you can make to begin a gluten-free diet. What are your favorite gluten-free items? Let me know if you’re following this diet and if it has helped you in any way!
Original blog may be found directly on Shawn's site here!
Stay connected with Shawn Wells:
- Instagram @ingredientologist
- Facebook /Ingredientologist
- LinkedIn /zonehalo
- shawnwells.com
Want to be featured by ICON Meals? Submit your stories to info@iconmeals.com or send us a DM on IG or Facebook!
REFERENCES
- Sharma N, Bhatia S, Chunduri V, et al. Pathogenesis of Celiac Disease and Other Gluten Related Disorders in Wheat and Strategies for Mitigating Them. Front Nutr. 2020;7:6. Published 2020 Feb 7. doi:10.3389/fnut.2020.00006 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7020197/
- Parzanese I, Qehajaj D, Patrinicola F, et al. Celiac disease: From pathophysiology to treatment. World J Gastrointest Pathophysiol. 2017;8(2):27-38. doi:10.4291/wjgp.v8.i2.27 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5437500/
- APA Howdle, Peter D. Gliadin, glutenin or both? The search for the Holy Grail in coeliac disease, European Journal of Gastroenterology & Hepatology: July 2006 – Volume 18 – Issue 7 – p 703-706 doi: 10.1097/01.meg.0000221847.09792.34
- https://www.mayoclinicproceedings.org/article/S0025-6196(15)00589-3/fulltext
- Saturni L, Ferretti G, Bacchetti T. The gluten-free diet: safety and nutritional quality. Nutrients. 2010;2(1):16‐34. doi:10.3390/nu20100016 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3257612/
- Di Sabatino A, Corazza GR. Nonceliac gluten sensitivity: sense or sensibility?. Ann Intern Med. 2012;156(4):309‐311. doi:10.7326/0003-4819-156-4-201202210-00010 https://pubmed.ncbi.nlm.nih.gov/22351716/
- Vazquez-Roque M, Oxentenko AS. Nonceliac Gluten Sensitivity. Mayo Clin Proc. 2015;90(9):1272‐1277. doi:10.1016/j.mayocp.2015.07.009 https://pubmed.ncbi.nlm.nih.gov/26355401/
- Leonard MM, Sapone A, Catassi C, Fasano A. Celiac Disease and Nonceliac Gluten Sensitivity: A Review. JAMA. 2017;318(7):647‐656. doi:10.1001/jama.2017.9730 – https://pubmed.ncbi.nlm.nih.gov/28810029/
- Naik RD, Seidner DL, Adams DW. Nutritional Consideration in Celiac Disease and Nonceliac Gluten Sensitivity. Gastroenterol Clin North Am. 2018;47(1):139‐154. doi:10.1016/j.gtc.2017.09.006 https://pubmed.ncbi.nlm.nih.gov/29413009/
- Niland B, Cash BD. Health Benefits and Adverse Effects of a Gluten-Free Diet in Non-Celiac Disease Patients. Gastroenterol Hepatol (N Y). 2018;14(2):82-91.
- Saturni L, Ferretti G, Bacchetti T. The gluten-free diet: safety and nutritional quality. Nutrients. 2010;2(1):16‐34. doi:10.3390/nu20100016 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3257612/
- Fric P, Gabrovska D, Nevoral J. Celiac disease, gluten-free diet, and oats. Nutr Rev. 2011;69(2):107‐115. doi:10.1111/j.1753-4887.2010.00368.x https://pubmed.ncbi.nlm.nih.gov/21294744/
- de Punder K, Pruimboom L. The dietary intake of wheat and other cereal grains and their role in inflammation. Nutrients. 2013;5(3):771-787. Published 2013 Mar 12. doi:10.3390/nu5030771
- https://www.glutenfreesociety.org/guidelines-for-avoiding-gluten-unsafe-ingredients-for-gluten-sensitivity/
- https://www.healthline.com/nutrition/gluten-free-foods#14